Welcome to the
(Video) Library

REAL PHYSICIAN EXPERIENCES WITH LIVMARLI
Meet real physicians and key experts who share their experiences and offer their perspectives on everything from patient diagnosis to treatment with LIVMARLI.


Physicians’ Perspectives on Pruritus
Listen in as Dr Jennifer Vittorio and Dr Saeed Mohammad reflect on their experiences treating patients with cholestatic pruritus.
Chapters








[00:00:00] [music]
Jennifer Vittorio: My name is Dr Jennifer Vittorio and I’m a pediatric hepatologist.
Saeed Mohammad: I’m Dr Saeed Mohammad, and I’m a pediatric hepatologist.
Jennifer: What if I asked, what does your patient population look like?
Saeed: I’m starting to see a lot more kids with genetic liver disease. [00:00:30] Things like Alagille syndrome, and then some of the more…I’d say, more rare liver diseases now that we’re doing more genetic testing.
Jennifer: Right, earlier on.
Saeed: Yes. What about you?
Jennifer: To be honest with you, we do have a large Alagille population where we’re practicing, but they’re presenting with cholestasis. They’re being referred to us, more so with the idea of we want to make sure that this is not a biliary atresia patient where, of course, timely diagnosis is critical. [00:01:00]
[music]
Jennifer: I don’t know about you, but what are some of the things that you think are most challenging about these patients? Because for me, I’m seeing a lot that are developing symptoms of pruritus over time. That just seems to be one of the hardest things to not only treat, but to identify.
Saeed: I think pruritus is so difficult. A lot of these kids [00:01:30] who are 3 or 4 months old, they’ll be maybe irritable or fussy, or parents will often go to their pediatrician and just say, “They’re more fussy.” What 3 or 4 month old isn’t fussy?
Jennifer: Isn’t fussy, yes.
Saeed: I think it becomes really hard to identify.
Jennifer: One of the things I’ve been really trying to do is to introduce the education of signs and symptoms a little bit earlier on. Certainly, when you’re meeting families for the first time, and you’re discussing [00:02:00] the diagnosis, focusing not only on the liver, and, “Here are some of the things that we may talk about further over time.” On subsequent visits, we’re seeing them for weight checks and monitoring their liver function tests. I’m really trying—and this is something that I’ve changed in my practice—is trying to talk about what does itchiness, what does pruritus look like?
Because I think especially for the young ones, like you mentioned, irritability, maybe waking up in the middle [00:02:30] of the night. I find that asking them about sleep is a great question. I get a lot of families who say, “Oh, I think they’re just hungry, and I give them the bottle, but lately they haven’t been falling back to sleep.” I think sometimes those are small clues that maybe there’s a little bit more going on.
Saeed: What about toddlers? What do you see with toddlers? Do you see the typical itching more?
Jennifer: I think you start to see maybe some of those scratch marks, and so there can be some findings on the skin. During the daytime, there’s a lot of distraction but at night, [00:03:00] when those distractions go away, I think is really when their symptoms are more prominent and troublesome.
Saeed: Yes. I think we see a lot in the ears, like they’ll scratch their ears so much they’re bleeding, their nose, face. People say it’s just itching, but you can get infections from it. Then, in those kids who are starting to go to school, I think they’re also, their school performance is affected.
Jennifer: They just can’t sit, they can’t pay attention. Because when you’re feeling that way, how can you [00:03:30] be expected to sit down and pay attention in school?
Saeed: In teenagers, I find that they’ve often normalized the itch. They might not complain as much, but they also have irritability, mood changes. Some of them are more withdrawn than normal, so they don’t want to take part in the usual, maybe teen activities because they don’t want to be outside. They don’t want to be seen itching. They don’t want to seem different. Itching is not just scratching your skin, it’s all those things that you said about [00:04:00] fidgeting, school performance, not sleeping at night, irritability, thinking they have ADHD, fatigue.
[music]
Saeed: We do a lot of blood testing for liver numbers, bilirubin, and we can do a physical exam to listen for stuff, but Itching is just…There’s no great test for it.
Jennifer: There’s no test for it, and a lot of times, we’re relying on the caretakers. [00:04:30] We’re seeing them in the office for a snapshot of their day, but we don’t know what’s happening overnight, we don’t know what happens when they walk out the door.
Saeed: I used to put more stock in, like, “Oh, they weren’t itching in front of me, so they’re probably not itching as much.” Now, I think I’m trying to change a little bit more to ask the parents or caregiver, like, “What do you guys think? What are you seeing? Do you see any improvement? Do you see any changes?” I think some of that change in me [00:05:00] has come from looking at and listening to some materials from some of these national groups like The Alagille Alliance. I think they’ve been really great at promoting education about what kids or what families with Alagille go through.
[music]
Jennifer: For me, I think my practice has evolved in the last couple of years. Most of the time, especially [00:05:30] for the young ones, while we’re working them up, as we’re trying to make a diagnosis, I would say a lot of times they end up on some choleretic agent like ursodiol. Oftentimes they’re starting there, but then despite that, they’re developing symptoms. In the past, I think I was quick to go to things like rifampin, maybe even-
Saeed: Antihistamines.
Jennifer: -antihistamines, but to be honest with you, I really hate those, because then I have kids who come to the office [00:06:00] and they’re sleepy and they’re struggling to stay awake sometimes. If they are school-aged, that’s also problematic. Again, when we’re talking about pruritus, I think it was a little bit less aggressive or forthcoming in asking about pruritus because I just felt like all we were doing was just increasing doses or adding different medications-
Saeed: It didn’t even work.
Jennifer: -and it wasn’t helping. Then you’re talking about, “What are the next steps?” Is it subjecting someone to an invasive procedure like a surgery, [00:06:30] either a bypass surgery or even liver transplant?
Saeed: You don’t take transplant lightly.
Jennifer: No.
Saeed: If you just say it, “Oh, I’m transplanting somebody for itching,” people will think you’re crazy. But if you see what it is, itching is not just scratching your skin.
[music]
Saeed: [00:07:00] Now that we have LIVMARLI to treat patients with cholestatic pruritus, how has that changed your practice?
Jennifer: I think it’s definitely impacted my treatment algorithm for pruritus. For those that I’ve never really been able to provide them with any significant relief, I’m talking to them and I’m introducing LIVMARLI almost immediately at this point. In some cases, I’ve really noticed some pretty impressive improvements [00:07:30] in about like 3 or 4 weeks or so. I think what has changed the most is for patients that I’m meeting with a new diagnosis of Alagille.
I think now I’m pretty quick to introduce LIVMARLI in my treatment algorithm, rather than waiting and trying a few of the medications that I’m more accustomed to, but it’s been working out really well.
[music]
Saeed: [00:08:00] Alagille is a rare disease, so it takes a while to get a brand new diagnosis. I have picked up the care of a few older patients. When I first met one of them, they were not doing well in school because they were itching a lot and were missing a lot of school. But they didn’t really bring up itch as a problem. They didn’t recognize it. When I see somebody on 3 medications for itch, even if they’re not complaining about it, I think [00:08:30] something must be going on.
Jennifer: There’s got to be a reason.
Saeed: There has to be a reason why they’re on it. I started that patient on LIVMARLI, and within a month, they were feeling much better. I’ve started to take them off those other medications-
Jennifer: Some of the other ones.
Saeed: -and they’re still remaining asymptomatic.
[music]
Saeed: In the past, one of the things that we didn’t maybe talk enough about was the cholestatic pruritus because we couldn’t fix it. [00:09:00] Even though I wanted to know about it, I knew there was nothing that I could do. I had them on maximum medication, and then the next step would have been maybe an antidepressant or surgical diversion, that kind of thing. I think also what we have to educate families about is that they have to keep telling us. If you tell me, “My child is itching,” and I don’t offer you anything, [00:09:30] after a while, you’re going to stop.
I think there was a time, or there’s a lot of patients who stopped stating or complaining about the itch, and a lot of physicians who also stopped asking because we were both like, “There’s nothing else we can do. It happens.”
Jennifer: You feel like you failed them, and you don’t want to keep calling that to attention almost.
Saeed: Yes. You don’t want to bring up your failure, but now, with LIVMARLI, and the efficacy I’ve seen with it, I tell other, either pediatricians or even other pediatric GI people that, “We do have a medication that can help with pruritus.” To me, it doesn’t matter what level of pruritus it is. Any itch can be treated. I wouldn’t wait until it’s severe. I don’t think it’s fair to make a kid miserable, and then give them the medicine that works, especially one that has [00:10:30] so few side effects.
Jennifer: Side effects, yes.
[music]
Jennifer: I have had a few patients who have had some increase in diarrhea. It makes sense when we think about the mechanism of action, we’re trying to increase fecal excretion of bile acids, rather than sending them back to an already overwhelmed liver, so to speak. What I’ve found for the most part is that those side effects are transient. [00:11:00] They maybe last a couple of days when we’re first introducing the medication, and in most instances get better.
Saeed: I’ve had abdominal pain for a few days that resolved, and I’ve had diarrhea for a few days that also resolved, and they continue taking the medicine. I think that, for me, the side effects profile has been really favorable. I’ve had a really good experience with the [00:11:30] Access Program. There’s a form that you have to fill, and you send it over to them. My patients have gotten medication very quickly. The approval has been pretty fast.
The thing I appreciate the most is they will follow up with me and say, “The patient needs a refill or the patient is not filling the medication.” They keep track of the medication. I know if the patient is taking it or not, so that when they come back to see me, I have an idea [00:12:00] about whether it’s working or not, and what do I have to talk to them about.
[music]
Saeed: I think the most important piece of advice I would give other physicians who treat cholestatic pruritus in patients who have Alagille syndrome is to keep an open line of communication with the caregivers and the parents so that they tell you exactly what’s going on. As we know, a lot of them may downplay the symptoms, and you might not get the whole picture about what’s happening [00:12:30] at home. The second part is that any level of itch or pruritus is probably too much. If we have the means to make things better, whether we consider it mild and they consider it moderate, I think, to me, it’s all the same. I would treat it with a medication that works.
[music]
Voiceover:
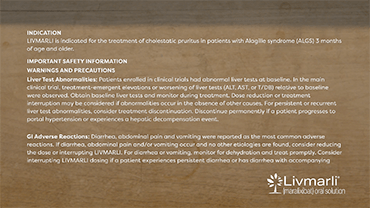
INDICATION
LIVMARLI is indicated for the treatment of cholestatic pruritus in patients who are 3 months of age and older with Alagille syndrome.
IMPORTANT SAFETY INFORMATION
CONTRAINDICATIONS
LIVMARLI is contraindicated in patients with prior or active hepatic decompensation events (eg, variceal hemorrhage, ascites, or hepatic encephalopathy).
WARNINGS AND PRECAUTIONS
Hepatotoxicity: LIVMARLI treatment is associated with a potential for drug-induced liver injury. In the Alagille syndrome trial, treatment-emergent elevations of liver tests or worsening of liver tests occurred.
Obtain baseline liver tests and monitor during treatment. Liver-related adverse reactions and physical signs of hepatic decompensation should also be monitored. Dose reduction or treatment interruption may be considered if abnormalities occur in the absence of other causes. For persistent or recurrent liver test abnormalities, consider treatment discontinuation. Permanently discontinue LIVMARLI if a patient experiences the following: persistent or recurrent liver test abnormalities, clinical hepatitis upon rechallenge, or a hepatic decompensation event.
Gastrointestinal (GI) Adverse Reactions: Diarrhea and abdominal pain were reported as the most common adverse reactions. Monitor for dehydration and treat promptly. Consider reducing the dosage or interrupting dosing if a patient experiences persistent diarrhea or has diarrhea with bloody stool, vomiting, dehydration requiring treatment, or fever.
Fat-Soluble Vitamin (FSV) Deficiency: Patients can have FSV deficiency (vitamins A, D, E, and K) at baseline, and LIVMARLI may adversely affect absorption of FSVs. If bone fractures or bleeding occur, consider interrupting LIVMARLI and supplement with FSVs. LIVMARLI can be restarted once FSV deficiency is corrected and maintained at corrected levels.
Risk of Propylene Glycol Toxicity (Pediatric Patients Less Than 5 Years of Age): Total daily intake of propylene glycol should be considered for managing the risk of propylene glycol toxicity. Monitor patients for signs of propylene glycol toxicity. Discontinue LIVMARLI if toxicity is suspected.
ADVERSE REACTIONS
The most common adverse reactions are diarrhea, abdominal pain, vomiting, FSV deficiency, liver test abnormalities, and bone fractures.
DRUG INTERACTIONS
Administer bile acid binding resins at least 4 hours before or 4 hours after administration of LIVMARLI. A decrease in the absorption of OATP2B1 substrates (eg, statins) due to OATP2B1 inhibition by LIVMARLI in the GI tract cannot be ruled out. Consider monitoring the drug effects of OATP2B1 substrates as needed.
DOSING INFORMATION
LIVMARLI should be taken 30 minutes before a meal. The provided oral dosing dispenser must be used to accurately measure the dose. Any remaining LIVMARLI should be discarded 100 days after first opening the bottle.
[music]
[00:16:30] [END OF AUDIO]
Root Out
Excess Bile
Learn how LIVMARLI—the first FDA-approved treatment for cholestatic pruritus in Alagille syndrome—battles bile acid buildup.1
See How LIVMARLI Works
Encourage patients to download the Itch✓ app to help them track symptom patterns over time and generate customized reports to share at appointments.
Check Out the Itch✓ App
Mirum Access Plus assists both you and your patients at every turn, helping you navigate the payer approval process—and beyond—with ease.
Learn More AboutMirum Access Plus

